Ankle injuries and fractures can significantly impact mobility and daily activities. Among the most severe types of fractures are trimalleolar ankle fractures and pilon fractures. Although both affect the lower extremities, they involve distinct anatomical structures, mechanisms of injury, and treatment approaches. Understanding the differences between these two fractures is crucial for accurate diagnosis, effective management, and successful rehabilitation.
Anatomy Involved in Trimalleolar Ankle Fractures and Pilon Fractures
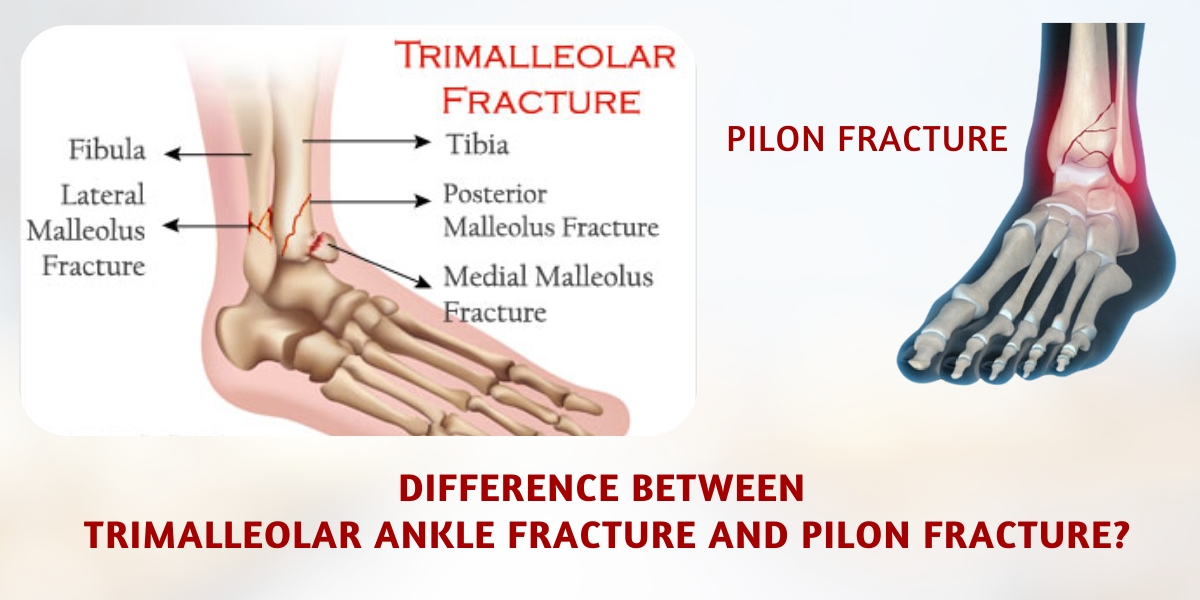
Trimalleolar Ankle Fracture
A trimalleolar ankle fracture involves three components of the ankle:
- The medial malleolus (the inner bone of the ankle).
- The lateral malleolus (the outer bone of the ankle).
- The posterior malleolus (the back portion of the tibia).
This type of fracture often results from high-energy twisting or rotational forces applied to the ankle joint, such as during sports injuries, falls, or automobile accidents. It disrupts the stability of the ankle joint, leading to significant functional impairment if not managed promptly.
Pilon Fracture
A pilon fracture, also known as a tibial plafond fracture, occurs at the distal end of the tibia, where it forms the roof of the ankle joint. Unlike trimalleolar fractures, pilon fractures involve both the tibia and, in some cases, the fibula. They result from high-energy impacts, such as falling from a height or motor vehicle accidents. The force of impact compresses the tibia into the talus, causing severe comminution (shattering) and damage to the surrounding soft tissues.
Mechanisms of Injury
Trimalleolar Ankle Fracture
- Rotational Trauma: Twisting injuries are the most common cause. Examples include slipping on uneven surfaces or sudden pivoting during sports activities.
- Direct Impact: A sudden blow or force to the side of the ankle may also cause trimalleolar fractures.
Pilon Fracture
- Axial Loading: Pilon fractures are typically caused by vertical forces, such as falling from a significant height, where the body’s weight drives the tibia downward into the talus.
- High-Energy Trauma: Automobile or motorcycle accidents frequently lead to these fractures due to the intense compressive forces involved.
Clinical Presentation
Trimalleolar Ankle Fracture
- Severe pain and swelling around the ankle joint.
- Visible deformity in severe cases.
- Inability to bear weight or move the ankle.
- Bruising and tenderness around the malleoli.
Pilon Fracture
- Intense pain and significant swelling extending up the leg.
- Often accompanied by open wounds or soft tissue damage due to high-energy trauma.
- Gross deformity in severe cases, with fragments of the tibia displaced.
- Restricted movement and inability to bear weight.
Radiological Diagnosis
Trimalleolar Ankle Fracture
X-rays in multiple views (AP, lateral, and oblique) are essential to visualize the fracture of the medial, lateral, and posterior malleoli. In complex cases, CT scans may be used to assess the fracture alignment and plan surgical intervention.
Pilon Fracture
A CT scan is often mandatory to evaluate the extent of the comminution and articular involvement. X-rays may initially reveal the fracture pattern, but the detailed imaging provided by CT helps determine the surgical strategy.
Treatment Approaches
Trimalleolar Ankle Fracture
- Non-Surgical Management:
- Reserved for minimally displaced fractures.
- Includes casting or bracing to immobilize the joint.
- Requires close monitoring with follow-up imaging.
- Surgical Intervention:
- Most trimalleolar fractures require open reduction and internal fixation (ORIF) to realign the bones and stabilize the joint.
- Hardware such as plates, screws, and wires are commonly used.
- Post-operative rehabilitation is critical to restoring ankle function.
Pilon Fracture
- Initial Management:
- Stabilization with a splint or external fixation to control swelling and maintain alignment.
- Address soft tissue injuries before definitive surgery.
- Definitive Surgery:
- ORIF is typically required to reconstruct the tibial plafond and restore joint congruency.
- In some cases, bone grafting is necessary to fill voids caused by comminution.
- Severe fractures may require arthrodesis (joint fusion) as a salvage procedure.
- Rehabilitation:
- Recovery often takes longer than for trimalleolar fractures due to the complexity and severity of pilon fractures.
- Weight-bearing restrictions may last several months.
Complications
Trimalleolar Ankle Fracture
- Post-Traumatic Arthritis: Damage to the cartilage can lead to long-term joint pain and stiffness.
- Malunion or Nonunion: Improper healing can result in deformity or chronic instability.
- Infection: Particularly in cases of surgical intervention.
Pilon Fracture
- Soft Tissue Damage: Extensive injuries increase the risk of infection and delayed healing.
- Arthritis: Joint surface irregularities can lead to early-onset arthritis.
- Nonunion or Malunion: The severity of the fracture increases the likelihood of these complications.
- Compartment Syndrome: High-energy trauma can lead to increased pressure within the leg, compromising blood flow and nerve function.
Prognosis
Trimalleolar Ankle Fracture
- With proper treatment, most patients regain functional mobility within 3–6 months.
- Long-term outcomes are favorable with minimal complications if surgery and rehabilitation are done correctly.
Pilon Fracture
- The prognosis is more guarded due to the complexity of the fracture and the involvement of the soft tissues.
- Full recovery may take 12 months or longer, depending on the severity of the injury and the patient’s adherence to rehabilitation protocols.
Key Differences Between Trimalleolar Ankle Fractures and Pilon Fractures
| Feature | Trimalleolar Ankle Fracture | Pilon Fracture |
|---|---|---|
| Anatomy | Medial, lateral, and posterior malleoli | Distal tibia (tibial plafond) |
| Mechanism of Injury | Rotational or twisting trauma | High-energy axial loading |
| Severity | Less severe compared to pilon | More severe, often with soft tissue damage |
| Treatment | Often ORIF, quicker recovery | ORIF, external fixation, or arthrodesis, longer recovery |